Medical doctors and Surgeons
Minimally invasive solutions in abdominal wall surgery
Abdominal wall surgery is a crucial field in the treatment of conditions affecting the abdominal wall. In recent years, the number of surgeries for such conditions has been on the rise. «In 2022, approximately 17,000 patients with abdominal wall disorders were recorded» says Dr Alessandra Saputelli, General Surgeon and Medical Director at the UOC General and Emergency Surgery Department at San Filippo Neri Hospital
Abdominal wall disorders
Abdominal wall disorders can be classified as either primary or secondary. Primary disorders mainly include ventral, epigastric, or umbilical hernias. Secondary conditions are more common. They often present as incisional hernias (laparoceles), which are post-surgical complications arising from laparoscopic, robotic, or open surgery.
Incisional hernias, in particular, can occur in areas of reduced resistance in the abdominal wall, such as trocar access points. Factors such as excess weight or patient comorbidities can contribute to their formation.
«If the fascia has not been properly repaired or if the patient has gained weight, combined with significant comorbidities, incisional hernias can form at trocar sites», adds Dr Saputelli.
Before undergoing abdominal wall surgery, the patient must be properly prepared. Taking into account any existing comorbidities, such as smoking, diabetes, or respiratory and cardiac issues.
«At San Filippo Neri, we have a technical and assistance protocol for pre-operative preparation to reduce complications before and after surgery. We work with physiotherapists and physiatrists who help patients avoid using their abdomen during various movements or normal daily activities. Specialists such as diabetologists, nutritionists, pulmonologists, and cardiologists support patients with these comorbidities, ensuring they are in optimal condition for surgery», explains Dr Saputelli.
The diagnosis of abdominal wall disorders is generally made using a CT scan without contrast. Conducted both at rest and during straining. This examination helps evaluate the size of the defect, the contents of the hernial sac, and the volume of the hernia itself. Based on these parameters, the most suitable surgical technique is chosen, reducing the risk of recurrence.
Classification criteria for incisional hernias

Surgical techniques for the abdominal wall vary depending on the type and severity of the condition. Smaller hernias can be treated using minimally invasive approaches, such as laparoscopic or robotic surgery. For more complex incisional hernias, instead, especially those exceeding 9 cm, open surgery remains the preferred option.
Minimally invasive approaches are generally more appealing to patients than a midline incision. However not all procedures can be performed using this technique. This is particularly the case for abdominal wall diastases greater than 9 cm.
«The classification of incisional hernias falls into three main categories: those under 4 cm, those between 4 and 10 cm, and those exceeding 10 cm, which represent a severe abdominal wall defect. In the latter case, the wall loses its function of containing abdominal contents, supporting the patient in an upright position, and aiding in respiratory compliance», explains Dr Saputelli.
Addressing diastasis with abdominal wall surgery
While pure diastasis falls under the remit of plastic surgeons, if associated with hernias, surgery is performed using laparoscopic or robotic techniques depending on the location of the hernia. Minimally invasive approaches are preferred to simultaneously treat diastasis and hernias.
«If umbilical or epigastric hernias are not associated with rectus diastasis, we can propose either open or laparoscopic techniques. Robotic surgery is used for abdominal wall disorders, such as umbilical and epigastric hernias, as well as for treating incisional hernias in their entirety. This approach, like laparoscopic surgery, reduces postoperative comorbidities more effectively than reducing operative time», notes Dr Saputelli.
Minimally invasive approaches not only provide satisfactory clinical outcomes but also offer significant psychological benefits for patients.
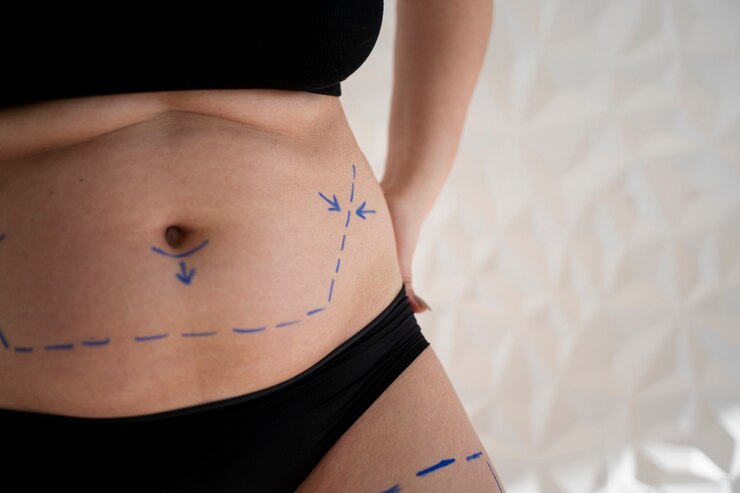
The absence of large scars and the potential for quicker recovery greatly improve postoperative quality of life. Patients are more likely to accept surgery when «techniques are explained to them. A three-trocar approach, with one 5 mm trocar and two 10-12 mm trocars, is far more acceptable than a midline incision», continues Dr Saputelli.
The use of robotic surgery, when applicable, represents a significant innovation. It expands the possibilities of minimally invasive procedures even in complex cases where traditional laparoscopy proves less effective.




































